- Research article
- Open Access
- Published:
Resident perspectives on the value of interdisciplinary conference calls for geriatric patients
BMC Medical Educationvolume21, Article number:314(2021)
Abstract
Background
There are limited competency-based educational curricula for transitions of care education (TOC) for internal medicine (IM) residency programs. The University of Colorado implemented a virtual interdisciplinary conference call, TEAM (Transitions Expectation and Management), between providers on the inpatient Acute Care of the Elder (ACE) unit and the outpatient Seniors Clinic at the University of Colorado Hospital. Residents rotating on the ACE unit participated in weekly conferences discussing Seniors Clinic patients recently discharged, or currently hospitalized, to address clinical concerns pertaining to TOC. Our goals were to understand resident perceptions of the educational value of these conferences, and to determine if these experiences changed attitudes or practice related to care transitions.
Methods
We performed an Institutional Review Board-approved qualitative study of IM housestaff who rotated on the ACE unit during 2018–2019. Semi-structured interviews were conducted to understand perceptions of the value of TEAM calls for residents’ own practice and the impact on patient care. Data was analyzed inductively, guided by thematic analysis.
Results
Of the 32 IM residents and interns who rotated on ACE and were invited to participate, 11 agreed to an interview. Three key themes emerged from interviews that highlighted residents’ experiences identifying and navigating some of their educational ‘blind spots:’ 1) Awareness of patient social complexities, 2) Bridging gaps in communication across healthcare settings, 3) Recognizing the value of other disciplines during transitions.
Conclusions
This study highlights learner perspectives of the benefit of interdisciplinary conference calls between inpatient and outpatient providers to enhance transitions of care, which provide meaningful feedback and serve as a vehicle for residents to recognize the impact of their care decisions in the broader spectrum of patients’ experience during hospital discharge. Educators can maximize the value of these experiences by promoting reflective debriefs with residents and bringing to light previously unrecognized knowledge gaps around hospital discharge.
Background
In an era of rising costs of health care, increasing attention is being placed on improving the quality of care at hospital discharge in order to avoid readmissions and other adverse patient outcomes. Multiple components contribute to an ideal transition of care (TOC) following hospitalization, including communication of information, medication safety, optimization of community resources, patient education, care coordination across team members, and monitoring/managing symptoms after discharge [1].Over the past several years, multiple programs have been developed and evaluated to improve transitions of care for older adults [2,3].In one recent study, the Extension for Community Health Outcomes-Care Transitions (ECHO-CT), a novel program involving interdisciplinary videoconferences for transitions of care was implemented for providers to discuss post-hospitalization skilled nursing facility (SNF) patients. This program led to a significant improvement in 30-day hospital readmissions, SNF length of stay, and 30-day total health care costs for patients [4].然而,综合通信acr的模型oss sites of care have not been widely adopted, and many academic centers rely on written materials alone to bridge the gap between sites of care.
In 2012, the Alliance for Academic Internal Medicine (AAIM) Education Redesign Subcommittee proposed Entrustable Professional Activities (EPAs) for residency programs to achieve competency-based educational goals for residents, mandated by the Accreditation Committee of Graduate Medical Education (ACGME) [5,6].Despite EPA’s inclusion of educational goals like transitions of care and leading and working within an interprofessional health care team, few models exist to guide post-graduate curricula in these areas.
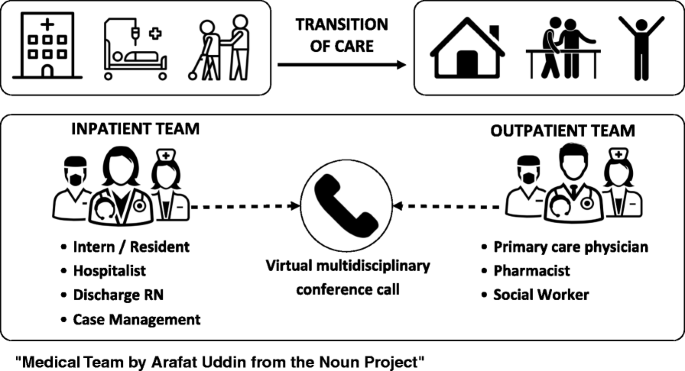
转换前的护理课程学生ied for their effect on clinical and patient-centered outcomes, but few studies have sought to better understand resident perceptions of these programs [7,8].In 2018, we implemented and adapted the ECHO-CT model to include weekly virtual interdisciplinary conference calls, referred to hereafter as Transitions Expectation and Management (TEAM) calls, between interprofessional providers on the geriatric inpatient unit of the University of Colorado Hospital and the Seniors Clinic (See Fig.1). The goal of TEAM calls was to improve coordination around care transitions and to improve resident transitional care education. We completed a qualitative descriptive study to understand the perceived educational value of the interdisciplinary TEAM calls from the perspective of internal medicine interns and residents.
Methods
Design and setting
This is a qualitative descriptive study of resident experiences with weekly TEAM meetings on the Acute Care of the Elder (ACE) inpatient unit of an urban quaternary care academic medical center. As part of clinical rotations, internal medicine residents rotate on geriatric general medicine ward teams on the 21-bed ACE Unit, which specializes in the care of patients over 72 years of age. In September 2018, ACE unit leadership implemented new interdisciplinary weekly virtual TEAM calls between members of the inpatient ACE clinical service along with interprofessional staff of the outpatient geriatrics clinic (UCHealth Seniors Clinic) to discuss currently admitted and recently discharged mutual patients. Inpatient ACE team representatives on the calls included residents, the attending physician from the inpatient team, and the transitions of care nurse. Seniors Clinic representatives included members of the primary care provider team, social worker, nurses, and outpatient pharmacists. TEAM calls provided opportunities to clarify questions on medical care, identify risks to effective transition planning, and provide bi-directional feedback on effective execution of the intended plan and patient status following a transition of care. TEAM calls were facilitated using secure video conferencing to allow for real-time collaborative review of patient charts in the electronic medical record between both ACE and Seniors Clinic participants.
Participants
Semi-structured interviews were completed with University of Colorado internal medicine residents rotating on the ACE unit who participated in TEAM calls between September 2018 and May 2019. Residents who rotated on ACE during this study period included those pursuing categorical internal medicine residency, customized internal medicine primary care or hospitalist training tracks, as well as preliminary medicine internship for specialties.
Data collection
A convenience sampling strategy was employed as part of a larger program evaluation to determine the educational value of TEAM calls and understand learner perspectives on optimizing transitions of care curricula. All 32 internal medicine residents who participated in ACE-Seniors clinic conference calls between September 2018 and May 2019 were invited by email to participate in interviews [9,10].Up to three total emails were sent to residents to invite participation. A semi-structured interview guide (see Additional file1) was used and included topics related to residents’ perceptions about the educational value of the TEAM calls to their own career trajectory, perceived time commitment, and impact on patient care from the calls. Individual interviews lasted up to 30 min and were completed either in person or over the telephone, per resident preference. The interviewer (BD) had prior experience conducting qualitative interviews and had no direct supervisory role for residents. Informed consent was completed prior to interviews, and participants were compensated $25 for interview completion. Interviews were audio recorded, professionally transcribed, and de-identified. This study was reviewed and deemed exempt by the Colorado Multiple Institutional Review Board.
Data analysis
The team (SJ, CJ, RN, TO) used an inductive approach to first read a small set of transcripts individually and design a code book together, which was refined over time as the team met and iteratively reviewed codes to establish consensus. Each of the interview transcripts was then coded in Atlas.ti (Version 7, Berlin, Germany) by at least two coders using open coding guided by thematic analysis, and emerging themes were identified [11,12].A record of all analytical decisions and team discussions was maintained. Triangulation was conducted with peers practicing in hospital medicine (EC, CJ, RN) and geriatric medicine (TO) to enhance reliability [13].
Results
We conducted 11 interviews with internal medicine residents who rotated on the ACE unit during 2018–2019. Of the residents interviewed, two were first-year intern residents, seven were in their second year, and two were in their third year. Four participants identified as female (36%). Seven interviewees were part of the Hospitalist Training Program within the residency, three were in the categorical track, and one was a preliminary resident.
Residents largely related their experiences on TEAM calls to their shared experience navigating educational ‘blind spots’ that they became aware of during their residency. These areas were commonly indicated by residents describing instances where “I didn’t know that” and “I never knew …” Interviews reflected a growing sense of awareness of the meaning and purpose underlying aspects of the work of managing transitions for complex vulnerable patients. One third-year resident explained how their attitude toward participating in the ACE-Seniors calls had evolved over time:
Initially it was a little like one extra thing they’re making us do, but as the weeks went on, I recognized that it was an important part in transitions of care and is something that I feel strongly can be a source of problems for patients when things get missed.
三个关键主题,进一步证明awareness of educational value of the calls and residents’ ability to identify and reconcile these newfound ‘blind spots’ in their training and education: gaining awareness of patient social complexities, bridging gaps in communication across different health care settings, and recognizing the value of other disciplines during transitions. Data relating to these themes are represented in Table1.
Theme 1: Awareness of patient social complexities
Residents shared insights into socioeconomic complexities uncovered during TEAM conferences. They commented on how barriers to care became increasingly apparent from communication across disciplines and healthcare settings, including patients’ ability to afford medication, stability of patients’ home lives, and high risk of readmission with inadequate resources upon discharge. One first-year resident explained:
[ACE] puts you into a position where you’re not just thinking of the patient’s survival needs for a few days. You really have to try to see bigger — their overall care. Being more responsible for discharge … your job isn’t just to get them out of the hospital but to make sure that when they are discharged, they have the correct follow up, they can afford the prescriptions in the plan that you’re discharging with, the medications can be afforded and continued …
Another first-year resident demonstrated new appreciation of the importance of effective transitions of care planning, especially in older patients:
The whole rotation cemented in my mind how difficult transitions of care are and how risky they are, especially in the older population.
A second-year resident further expressed how TEAM calls prompted them to proactively identify potential causes for readmission and address those prior to discharge:
It was really good to see in a more real-world setting how their follow up takes place outside of the hospital — understanding the gaps people fall into and understanding appropriate ways to communicate to try and avoid those for patients across the board.
Theme 2: Bridging gaps in communication across healthcare settings
Residents shared how TEAM calls reframed their perspectives on patients’ disparate experiences throughout different healthcare settings, helping them better contextualize their role within the larger order of patients’ movements through the healthcare system. A second-year resident specifically described a shift toward a more team-based approach between inpatient and outpatient providers:
You realize how much of an opportunity there is for you to be able to help other physicians, it’s just a reminder that my role is part of a continuum of care, and I need to be thinking about what ways I can contribute to that continuum and how I’m setting my colleagues up for success on the outpatient setting.
Another second-year resident felt that the direct communication with outpatient providers through TEAM calls also proved a valuable form of feedback beneficial for their own future practice:
Getting that outpatient perspective, what’s actually happening with this patient, was helpful in terms of informing the way that I thought about other patient encounters.
Residents recognized how TEAM calls framed their own perceptions of their position amidst transitions of care and reiterated their responsibilities and ability to improve transitions.
Theme 3: Recognizing the value of other disciplines during transitions
居民reflected on the value of interdisciplinary care during transitions. Acknowledging the importance of pharmacy involvement was common, with many trainees appreciating an added layer of oversight to reduce medication errors after discharge. Residents also noted the importance of social work and case management in facilitating “the care of the patient as an individual.” One second-year resident shared, “they’re really the ones who are specializing in care transitions and are especially knowledgeable about geriatric patient transitions.” Another second-year resident stated,
I didn’t know that pharmacy and social work were so intertwined in the post discharge care, so I thought that was really helpful that there was a chance to hand off to those people as well, in addition to just their provider.
However, some residents raised potential drawbacks with concern that “Sometimes there were too many cooks in the kitchen,” (second-year resident) especially if they did not have prior experience with interdisciplinary care or a framework to guide interactions between professions:
I think a lot of times we just throw a lot of specialties in the same place and think that it’s going to magically change the outcome, but I don’t know what the pharmacist needs from me or what specific questions I can help them with, where I have unique value … or the outpatient nurse or PT or social work. (Second-year resident)
重要的是要注意,虽然大多数居民reported perception of clinical value delivered by TEAM calls, some residents described contradictory attitudes or feelings about the educational value. One second-year resident stated, “I was already aware that it was very important to be very deliberate and clear with our discharge instructions”. Another second-year resident expressed similar sentiments in their position as a senior resident but recognized potential value of participation for interns:
I think it did help my interns a couple times because it highlighted near misses. Maybe they weren’t aware that they had to do it this way for this to be articulated, or maybe they had to re-write the ways that they wanted the medications to be taken. I think it definitely benefited the intern, but I don’t know that it changed the way that I would discharge a patient.
Discussion
We found that TEAM calls prompted a dawning awareness of residents’ educational blind spots related to transitions of care in elderly patients discharging from the hospital, especially related to residents’ increased appreciation of social factors that can affect health outcomes at discharge, perceptions of their role in patient care within the larger healthcare system, and valuation of a interdisciplinary approach at discharge. Considered together, the three key themes suggest a larger shift from an individualistic to a team-based approach on the part of the resident coordinating patient care after discharge.
医学院学生交易nsitions curricula consisting of didactics, experiential learning, and small group discussions have been studied previously [14,15,16], with one study observing increased awareness of challenges to effective discharge planning, as well as shifting attitude toward a more patient-centered approach [16], similar to our TEAM model in residents.
A limited number of groups have studied how TOC curricula impact resident perceptions of patient care around hospital discharge [7,8,17].One intervention integrated didactics with post-discharge follow up at skilled nursing facilities, nursing homes, and home health nursing visits [7].In another study, chart reviews of previously hospitalized patients were used as a way for residents to reflect on their practice and understanding of their patients’ needs [8].A third study involved experiential learning, self-learning by reading an article on TOC [2], facilitated small-group discussions, and writing a self-reflective essay [17].Several themes consistently emerged in this prior research: the importance of improved TOC planning [7,8,17], the importance of effective communication with receiving providers [7,8,17], with patients and families [8,17], and appreciation of social factors that impact safe discharge planning [18].These themes correlate with those that were evoked by TEAM calls.
Notably, participating in TEAM calls prompted residents to place higher value on other disciplines during transitions of care. Part of this is likely related to the design of the TEAM calls as interdisciplinary in nature. Interestingly, a TOC curriculum in which medical students and pharmacy students worked together to coordinate discharges and post-discharge follow up found a similar increase in appreciation of interdisciplinary care [15].Because a team approach is necessary to coordinate safe discharge planning, this suggests that future TOC interventions and curricula should incorporate an interdisciplinary focus with inclusion of other disciplines such as pharmacists, social workers and nurse case managers.
Key facilitators for the TEAM calls as an effective intervention included integration into normal clinical workflow for all participants, user-friendly teleconference interface, and a structured script to prompt participation for all inpatient and outpatient team members [18].These qualities, as well as the interdisciplinary nature of the calls adapted from the original ECHO-CT model, enhanced the sustainability of this model.
Implications
Overall, residents perceived value of participating in transitions of care TEAM calls that were designed to improve care coordination between inpatient and outpatient settings. Consistent with findings of a systematic review on physician training to provide “high-value, cost-conscious care,” transitions of care curricula should include 1) transmission of specific knowledge with didactics, 2) reflective practice, and 3) a supportive environment [19].Our TEAM model and other similar curricula consistently demonstrate a positive shift of resident attitude toward transitions of care with increased focus on a team-based approach across disciplines and sites to provide patient care.
Limitations
只有11 32邀请居民参加completed interviews and most were senior residents, likely reflective of busy clinical loads. Due to the voluntary nature of this study, our qualitative findings may not be reflective of all the residents who served on the Acute Care of the Elder unit. We continued recruitment until we reached thematic saturation, but we acknowledge that response bias is a limitation of our study. Only residents on the ACE service were interviewed; additional TEAM call participant interviews as well as patient and outpatient provider experiences may shed further light onto the utility of TEAM calls from other perspectives. TEAM calls may not be feasible to implement on inpatient services or clinics that lack adequate support staff or that have inadequate volume of patients cared for by the same inpatient and outpatient care teams.
Conclusion
TEAM calls provide residents with the opportunity for reflective experiential learning that highlights the importance of a team-based approach, involving multiple disciplines and sites of care, to maximize patient safety and success when discharging from the hospital. Methodical assessment of resident perceptions and attitudes toward TOC curricula can directly inform curricular improvements to optimize the value of resident education in this area. Our findings suggest that blind spots in resident understanding of effective transitions can be identified and addressed by interdisciplinary TEAM calls. Finally, our findings suggest the educational value of experiences with interdisciplinary TOC models may be promoted by reflective debriefs to illuminate previously unrecognized knowledge gaps.
Availability of data and materials
The dataset supporting the conclusions of this article are included within the article, in the text as well as the table/supplements. Given the nature of our qualitative interviews, and agreement with our local institutional review board (COMIRB), full interview transcripts/data are securely stored and not publicly available.
Abbreviations
- TOC:
-
Transitions of care
- ECHO-CT:
-
Extension for Community Health Outcomes-Care Transitions
- SNF:
-
Skilled Nursing Facility
- AAIM:
-
Alliance for Academic Internal Medicine
- EPA:
-
Entrustable Professional Activities
- ACGME:
-
Accreditation Committee of Graduate Medical Education
- TEAM:
-
Transitions Expectation and Management
- ACE:
-
Acute Care of the Elder
References
Burke RE, Kripalani S, Vasilevskis EE, Schnipper JL. Moving beyond readmission penalties: creating an ideal process to improve transitional care: moving beyond readmission penalties. J Hosp Med. 2013;8(2):102–9.https://doi.org/10.1002/jhm.1990.
Coleman EA, Parry C, et al. The Care Transitions Intervention: Results of a Randomized Controlled Trial. Arch Intern Med. 2006;166:7.
Kane RL, Huckfeldt P, Tappen R, Engstrom G, Rojido C, Newman D, et al. Effects of an intervention to reduce hospitalizations from nursing homes: a randomized implementation trial of the INTERACT program. JAMA Intern Med. 2017;177(9):1257–64.https://doi.org/10.1001/jamainternmed.2017.2657.
Moore AB, Krupp JE, Dufour AB, Sircar M, Travison TG, Abrams A, et al. Improving transitions to Postacute Care for Elderly Patients Using a novel video-conferencing program: ECHO-Care transitions. Am J Med. 2017;130(10):1199–204.https://doi.org/10.1016/j.amjmed.2017.04.041.
Chan B, Englander H, Kent K, Desai S, Obley A, Harmon D, et al. Transitioning toward competency: a resident-faculty collaborative approach to developing a transitions of care EPA in an internal medicine residency program. J Grad Med Educ. 2014;6(4):760–4.https://doi.org/10.4300/JGME-D-13-00414.1.
Green ML, Aagaard EM, Caverzagie KJ, Chick DA, Holmboe E, Kane G, et al. Charting the road to competence: developmental milestones for internal medicine residency training. J Grad Med Educ. 2009;1(1):5–20.https://doi.org/10.4300/01.01.0003.
Miller RK, Keddem S, Katz S, Smith Z, Whitehouse CR, Goldstein K, et al. Intern transitions of care curriculum through Posthospital home and skilled nursing facility visits. J Grad Med Educ. 2018;10(4):442–8.https://doi.org/10.4300/JGME-17-00499.1.
Narayana S, Rajkomar A, Harrison JD, Valencia V, Dhaliwal G, Ranji SR. What happened to my patient? An educational intervention to facilitate Postdischarge patient follow-up. J Grad Med Educ. 2017;9(5):627–33.https://doi.org/10.4300/JGME-D-16-00846.1.
Patton M. Qualitative evaluation and research methods. 2nd ed. Newbury Park: Sage Publications; 1990.
Trotter RT 2nd. Qualitative research sample design and sample size: resolving and unresolved issues and inferential imperatives. Prev Med. 2012;55(5):398–400.https://doi.org/10.1016/j.ypmed.2012.07.003.
Creswell J. Qualitative inquiry and research design: choosing among five approaches. 3rd ed. Thousand Oaks: Sage; 2012. p. 472. Paperback. ISBN: 9781412995306
Fereday J. Eimear Muir-Cochrane. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2010;5(1):80–92.
Carter N, Bryant-Lukosius D, DiCenso A, Blythe J, Neville AJ. The use of triangulation in qualitative research. Oncol Nurs Forum. 2014;41(5):545–7.https://doi.org/10.1188/14.ONF.545-547.
Bray-Hall S, Schmidt K, Aagaard E. Toward safe hospital discharge: a transitions in care curriculum for medical students. J Gen Intern Med. 2010;25(8):878–81.https://doi.org/10.1007/s11606-010-1364-3.
Lai CJ, Nye HE, Bookwalter T, Kwan A, Hauer KE. Postdischarge follow-up visits for medical and pharmacy students on an inpatient medicine clerkship. J Hosp Med. 2008;3(1):20–7.https://doi.org/10.1002/jhm.264.
Ouchida K, LoFaso VM, Capello CF, Ramsaroop S, Reid MC. Fast Forward Rounds: an effective method for Teaching medical students to transition patients safely across care settings: FAST FORWARD ROUNDS: TEACHING TRANSITIONS OF CARE. J Am Geriatr Soc. 2009;57(5):910–7.https://doi.org/10.1111/j.1532-5415.2009.02203.x.
Pavon JM, Pinheiro SO, Buhr GT. Resident learning across the full range of core competencies through a transitions of care curriculum. Gerontol Geriatr Educ. 2018;39(2):144–59.https://doi.org/10.1080/02701960.2016.1247066.
琼斯,CD;辛格,年代;美元,英国航空公司;马库斯;Linnebur, S; Pearson, S; Hartley, K; Parnes, B; Hagman, J; Cumbler, E. “Improving the catch: innovative video conferences to enhance transitional care communication and resident education.” Abstract published at Hospital Medicine 2019, March 24–27, National Harbor, MD, Abstract 39.
Stammen LA, Driessen EW, Notermans CCVI, Scheele F, Stassen LPS, Stalmeijer RE. How do attending physicians prepare residents to deliver high-value, cost-conscious care? Acad Med. 2019;1.https://doi.org/10.1097/ACM.0000000000003051.
Acknowledgements
Not Applicable.
资金
This work was supported by a grant from the University of Colorado Hospital and School of Medicine Clinical Effectiveness and Patient Safety small grants program. Dr. Jones is supported by grant number K08HS024569 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Author information
Authors and Affiliations
Contributions
RN: Reviewed and contributed to coding of transcriptions, writing and submission of the manuscript, and performed literature review. TAO: Reviewed and contributed to coding of transcriptions, writing of manuscript including introduction and discussion section, and performed literature review. SJ: Analyzed transcriptions, created code book and compiled qualitative responses to inform thematic analysis, contributed to the Methods and Results section of the manuscript. BD: Integral in recruitment and performing qualitative interviews during study. Reviewed and edited the key components of the manuscript. EC: Mentor who performed coding of transcriptions and edits of the manuscript. CJ: Mentor involved in recruitment of participants, provided funding for coding and transcription, and performed coding of transcriptions and edits of the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Colorado Multiple Institutional Review Board (COMIRB) deemed this work as “Non-Human Subject Research”- Protocol number 19–0521, “Evaluation of Video Conferences to Enhance Transitional Care Resident Education,” in March 2019.
Consent for publication
Not Applicable.
Competing interests
The authors of this manuscript do not have competing interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Interview Guide
Rights and permissions
Open AccessThis article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Naderi, R., Oberndorfer, T.A., Jordan, S.R.et al.Resident perspectives on the value of interdisciplinary conference calls for geriatric patients.BMC Med Educ21, 314 (2021). https://doi.org/10.1186/s12909-021-02750-4
Received:
Accepted:
Published:
DOI:https://doi.org/10.1186/s12909-021-02750-4
Keywords
- Qualitative
- Transitions of care
- 居民教育
- Internal medicine
- Geriatric medicine